Myelodysplastic Syndrome: Silent Signals You Shouldn’t Ignore
Could your body be revealing signs of a serious blood disorder without your awareness? Myelodysplastic syndrome (MDS) can develop quietly, with subtle signals that are easy to miss. In this article, we highlight the warning signs you shouldn’t overlook and explain why noticing them early can help you take informed steps toward better health.Myelodysplastic syndrome affects thousands of Americans each year, yet many people remain unfamiliar with this complex blood disorder. The condition occurs when the bone marrow, responsible for producing blood cells, begins creating abnormal or immature cells that cannot function properly. These defective cells accumulate in the bone marrow and bloodstream, leading to various health complications that can significantly impact quality of life.
Myelodysplastic syndrome (MDS) is a group of bone marrow disorders in which the body does not produce enough healthy blood cells. Because changes develop gradually, the earliest signs can feel ordinary—tiredness after a busy week, a cold that lingers, a bruise you don’t remember getting. Recognizing patterns and understanding how MDS affects blood production can help you identify signals worth discussing with a clinician.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is myelodysplastic syndrome and who is at risk?
MDS occurs when bone marrow—the spongy tissue that makes blood cells—creates cells that are abnormal or do not mature properly. Over time, this leads to shortages of one or more blood cell types (cytopenias). MDS is more common in adults over 60, though it can occur at other ages. Risk increases with prior chemotherapy or radiation, long-term exposure to certain chemicals such as benzene, tobacco use, and specific inherited conditions that affect DNA repair. Some people develop MDS without a clear cause. Having risk factors does not mean someone will develop the condition, but they can help explain why a clinician may look more closely at persistent blood count changes.
What are the early warning signs of MDS?
Early symptoms often reflect which blood cells are low. When red blood cells are reduced (anemia), fatigue, weakness, shortness of breath on exertion, paleness, or lightheadedness may appear. Low white blood cells—especially neutrophils—can lead to frequent or prolonged infections, fevers without a clear source, or slow recovery from common illnesses. Low platelets can cause easy bruising, nosebleeds, bleeding gums, petechiae (tiny red or purple spots), or longer bleeding from minor cuts. Some people notice unintentional weight loss or decreased exercise tolerance. In many cases, the first clue is an abnormal complete blood count (CBC) during routine testing before symptoms are obvious.
Why do these symptoms often go unnoticed?
The signals of MDS are nonspecific and overlap with everyday issues like stress, poor sleep, minor viral infections, or the natural effects of aging. Fatigue is especially easy to misattribute to busy schedules or other health conditions such as thyroid problems, diabetes, or depression. Infections and bruising may appear sporadic, so patterns can be missed. Many adults also do not have frequent blood tests, allowing gradual changes in counts to go undetected. Because symptoms evolve slowly, people often adapt their activity level without realizing they are compensating for reduced blood cell function. Recognizing persistence, frequency, and combinations of symptoms can help distinguish everyday fluctuations from a developing blood disorder.
How does MDS affect your body’s blood production?
Healthy bone marrow continually produces red blood cells (carry oxygen), white blood cells (fight infection), and platelets (aid clotting). In MDS, immature cells do not mature correctly, and many die before leaving the marrow. This inefficient process—called ineffective hematopoiesis—leads to low numbers of functioning cells in the bloodstream. Anemia reduces oxygen delivery, causing fatigue and shortness of breath. Neutropenia weakens immune defenses, raising infection risk. Thrombocytopenia impairs clot formation, leading to bruising and bleeding. Under the microscope, marrow cells can appear dysplastic (abnormally shaped), and genetic changes in marrow cells are common. A subset of cases can evolve into acute myeloid leukemia, which is why careful monitoring and risk assessment by a hematology specialist are important.
When should you seek medical attention?
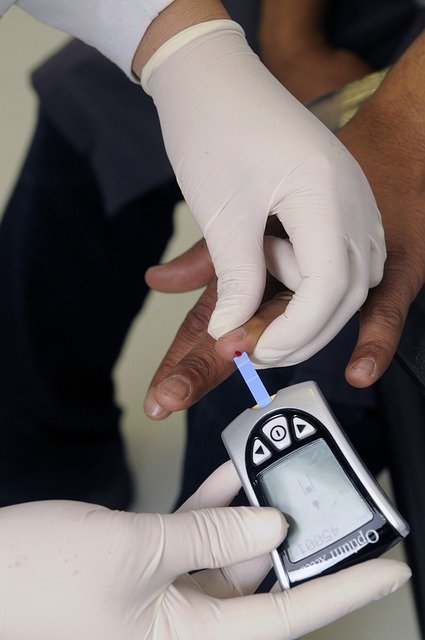
Consider medical evaluation if fatigue persists despite rest, you experience repeated infections or fevers, bruising or bleeding occurs more easily than usual, or shortness of breath limits normal activity. Seek prompt care for heavy or uncontrolled bleeding, chest pain, or high fever. If routine blood work shows unexplained anemia, low white blood cells, or low platelets, a clinician may repeat tests and investigate other causes such as nutritional deficiencies or chronic illnesses. Further workup can include a peripheral smear, reticulocyte count, iron, vitamin B12, and folate levels, and sometimes viral testing. If MDS is suspected, a hematologist may recommend a bone marrow biopsy to examine cell development and chromosomal changes. Early evaluation helps clarify the cause of symptoms and guides appropriate management and follow-up.
In summary, the signs of myelodysplastic syndrome are often subtle and gradual, which is why they can blend into daily life. Paying attention to persistent fatigue, recurrent infections, or unusual bruising—especially in the presence of risk factors—can prompt timely testing. Understanding how MDS disrupts the production of healthy blood cells provides context for symptoms and supports informed conversations with healthcare professionals.




